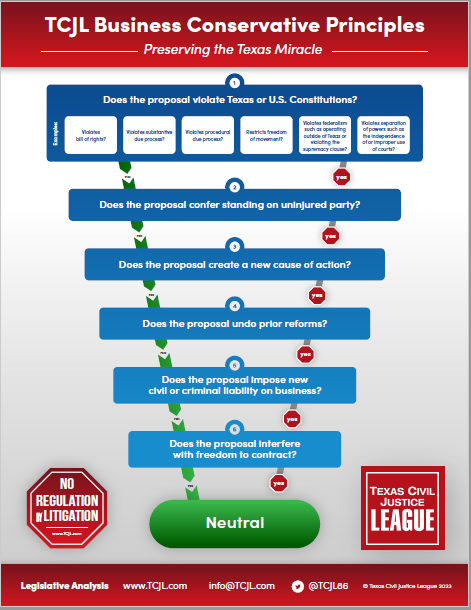
Twenty years ago this spring the Texas Legislature enacted and Governor Rick Perry signed HB 4, a series of medical liability reforms aimed at addressing a catastrophic liability insurance and access to care crisis stemming from medical malpractice lawsuits. Fast forward to 2023, where we are tracking dozens of bills that impose new liability on physicians and other health care providers in the form of private causes of action, statutory damages, unlimited punitive damages, civil and criminal penalties, and license revocation. Of course, we realize that most of these proposals will not get through the legislative process, but some of them undoubtedly will and the trend they may represent bodes ominously for the future.
Twenty years ago this spring the Texas Legislature enacted and Governor Rick Perry signed HB 4, a series of medical liability reforms aimed at addressing a catastrophic liability insurance and access to care crisis stemming from medical malpractice lawsuits. Fast forward to 2023, where we are tracking dozens of bills that impose new liability on physicians and other health care providers in the form of private causes of action, statutory damages, unlimited punitive damages, civil and criminal penalties, and license revocation. Of course, we realize that most of these proposals will not get through the legislative process, but some of them undoubtedly will and the trend they may represent bodes ominously for the future.
The Legislature has seen a lot of turnover since 2003, especially in the Texas House, so it may be useful to briefly review the situation that set the stage for HB 4 in the first place and what has happened since. Quoting our friends at Texas Alliance for Patient Access:
- “More than two-thirds of the state’s 22 trauma service areas experienced a per-population loss in direct patient care physicians during the liability crisis period. Since then, 80% of the state’s trauma service areas have experienced a per-population gain. During the crisis years, the number of new applicants and new licensees stagnated or declined. Since then, the number of new physicians applying for a Texas license is at an all-time high and the number of licenses granted continues at near record levels–growing even faster than our fast-growing population. Today, Texas has more patient care physicians per population than ever.”
- “During the post-crisis years, the number of high-risk specialists in Texas has grown more than twice as fast as the state’s population.”
- “During the two years prior to our reforms, 5,001 high-risk specialists limited their practice to less hazardous cases, meaning only 5,674 of 10,675 licensed high-risk specialists were actually providing a full range of services to patients. In short, Texans were finding fewer doctors to treat them when they needed expert care the most.”
- Passing tort reform reversed that trend. According to Texas Department of Insurance data, malpractice insurance rates have plunged more than 30 percent since passage, with some of the top insurers slashing rates more than 40 percent. As a result, Texas Medical Board data show the state has added 11,941 physicians since May 2003, a 31.3 percent surge, well above our population growth rate of 17 percent over that span. High-risk specialists are a big part of that trend, with their numbers growing more than twice as fast as the state’s population, and the number of pediatric sub-specialists growing at a rate 10 times faster.
- “Rural Texas was losing physicians per population during the liability crisis years. Today, those numbers are on the upswing. Since the passage of reforms, sixty-one rural counties have added at least one emergency medicine physician. Thirty-one rural counties have added an obstetrician. Twenty-one rural counties have added a cardiologist and seven have added an orthopedic surgeon. The rural gains are not simply a bi-product of population growth. For instance, forty-five rural counties that did not have a single emergency medicine physician in 2003 now do. Fourteen rural counties that lacked a cardiologist and twelve counties that lacked an obstetrician now have one.”
- “The Association of American Medical Colleges collects comparative data on physician supply in all 50 states. During the past six years, only California has added more patient care doctors than Texas. And remember, California’s population is 50% greater than that of Texas. Only Utah bested Texas in percentage growth. From 2008-2014, the most current years for which data is available, the Lone Star State ranked 20th in per-population physician growth; a remarkable accomplishment given our explosive population growth.”
- “Texas is adding new physicians faster than the population. Since 2003, the state has added 18,437 more in-state active physicians than can be accounted for by population growth alone. Population growth may well account for 41 percent of the state’s new physicians. The other 59 percent above the trend were produced by some other factors. Many of the state’s newly minted doctors have cited Texas’ more hospitable legal climate as a significant factor in their choosing to practice here.” https://www.tapa.info/texas-alliance-for-patient-access-physician-pre-post-reform.html.
Though the old saw that there are “lies, damn lies, and statistics” may be cited by those who disagree with the 2003 reforms, there can be no question that they delivered on their promise: to enhance access to care by reducing liability exposure for physicians, especially primary care physicians and those in specialties such as obstetrics and certain types of surgery. Simply stated, HB 4 worked.
While it is going too far to say that the 2023 version of the Legislature has turned away from HB 4 and the improvements we have seen in access to care, we believe that there is legitimate concern that proposals currently working their way through the process could reverse some of these gains, particularly in some of the areas where the pre-2003 crisis were most acute: primary care and obstetrics and gynecology. What is our evidence for this concern? Let’s review some of the proposals that we believe have the best chance of advancing this session.
HB 888. One of the most important of the 2003 reforms is found in § 74.251, CPRC. Prior to 2003, the statute of limitations in a medical malpractice claim involving a minor did not begin to run until the minor reached age 18. This resulted in “long tail” claims that could have (and were) brought against health care providers up to nearly two decades after the alleged malpractice occurred. Simply stated, no provider could insure this risk and, even if they could, would not have been able to afford it. Simply bringing the case would frequently result in a settlement because: (1) the provider had no effective defense to a claim alleging acts and omissions that allegedly occurred so far in the past, and (2) attempting to defend the claim would run the grave risk of bringing financial ruin upon the physician or provider, who might well have retired by the time suit was brought or otherwise be uninsured or underinsured. HB 4 addressed this problem by imposing a two-year limitations period on medical malpractice claims, establishing a 10-year statute of repose, and giving minors under age 12 until their 14th birthday to file their claims.
HB 888 create an exception to § 74.251 to extend the limitations period to the claimant’s 25th birthday if the claimant was a minor when the minor received a puberty suppressing drug, cross-sex hormone, or a surgical procedure or other treatment “for the purpose of gender transitioning or gender reassignment.” The bill thus not only reverses a prior reform and reintroduces “long-tail” liability exposure for certain treatments, it goes even further than the prior law, which at least required the claim to be brought by the minor’s 20th birthday. We suspect that this liability might fall most heavily on pediatricians and primary care physicians, whose efforts to provide the most effective treatment for myriad health conditions that might call for a particular drug, hormone, or other treatment will be rewarded by a lawsuit somewhere down the line. While it is perhaps true that a defendant physician could prevail in such a suit, the reality is not so simple. The reason HB 4 addressed long-tail liability in the first place was its crippling effect on the ability of health care providers to defend themselves from injuries that allegedly occurred in the increasingly distant past. At some point in the life of any claim, lapse of time and deterioration of evidence impairs the accuracy of fact-finding, encourages the assertion of fraudulent claims, increases the cost of litigation, and raises the chances of an erroneous and unjust result. This is the same risk that drove physicians out of the state prior to 2023, and reintroducing it here, albeit under somewhat limited circumstances (though the language of the bill is vague and will produce a lot of uncertainty on this point), is likely at the very least to have adverse unintended consequences.
SB 14/HB 1686. SB 14, which passed the Senate, bans certain medical procedures and treatments “for the purpose of transitioning a child’s biological sex . . . or affirming the child’s perception of the child’s sex if the perception is inconsistent with the child’s biological sex . . .” The bill authorizes the attorney general to enforce the prohibition by seeking injunctive relief. It also defines a prohibited procedure or treatment as a prohibited practice for purposes of physician licensing and mandates the revocation of a physician’s license if the physician provides such procedure or treatment (apparently without recourse or any other due process protections).
Setting aside the larger philosophical debate over whether state power should intervene in the relationship between a physician, a minor patient, and the minor’s parent or legal guardian in this fashion, the bill puts physicians and other health care providers at serious risk of liability in two ways: (1) for the direct provision of care to a child that the physician, the child, and the child’s parent or legal guardian deem necessary in his or her best medical judgment for the child’s health and well-being, and (2) for not providing treatment the physician, the child, and the child’s parent or guardian believe necessary, the absence of which leads to death or injury to the child. As we are already seeing in the abortion context, legal prohibitions of certain women’s health care procedures and treatments have created a widening gray area in which physicians and other providers must decide either to risk their professional and financial well-being (up to and including imprisonment) by treating a pregnancy-related complication or allowing the complication to worsen, threatening the health and life of the patient. It seems likely that a failure to treat a child for certain conditions associated with gender dysphoria could have a similar effect, leaving a physician damned for treating and damned for not treating. As the bill does not recognize the potential existence of the gray area or the legal limbo in which it maroons health care providers, the only thing left is a Hobson’s choice that hurts everyone involved.
HB 81/SB 177. These bills, both of which been heard in the respective House and Senate committees, make a health care provider liable for administering a COVID-19 vaccination, if the individual who received the vaccine “has been compelled or coerced into being vaccinated against COVID-19 contrary to the individual’s vaccination preference.” If found liable, the provider must pay at least $5,000 in statutory damages, plus court costs, attorney’s fees, investigation costs, witness fees, and deposition expenses. The bill further permits the recovery of punitive damages without meeting the standard of proof requirements of § 41.003, CPRC, or the requirement that plaintiff recover more than nominal damages as a prerequisite to recovery, as provided in § 41.004, CPRC.
It is difficult to get our mind around punishing a health care provider for what someone else may have done and for something the provider would neither have reason to suspect nor otherwise have any way of knowing anything about. This standard deviates from anything in our jurisprudence and, in essence, leaves a health care provider absolutely bare, with no defenses and no reasonable possibility of proving a negative (i.e., that the individual was not coerced into taking the vaccine). To make matters worse, the bill levies punitive damages without evidence of a tortfeasor’s actual malice, gross negligence, willful, wanton, or reckless conduct, or any other due process safeguards that the Texas Supreme Court and Legislature have put in place. We cannot imagine that any of this passes the smell test, much less constitutional muster, but here we are. We can only hope that reasonable minds prevail and this language comes out of the bill. But the fact that it is there and that both bills have received a hearing is both unsettling and indicative of a changing attitude toward the practice of medicine and traditional liability standards.
Beyond the specific ways in which these bills, and others like them, punish physicians and health care providers for practicing medicine in selected contexts, the bills, at least in our view, mark a potential sea change from the policy attitudes that led to the 2003 medical liability reforms and the subsequent success of the reforms. Whereas since 2003 policymakers have been wary of weakening or reversing the reforms (and have not done so), these bills clearly do. At the same time, proposals to safeguard the professional medical judgment of physicians in these and other contexts have not yet been heard and, for the most part, probably won’t be. There is no question that the state can regulate the practice of medicine; we have no issue with that. But when the state directs precisely whether and how a physician should or should not treat a scientifically recognized medical condition with serious health consequences to a patient, we have entered a new realm. That the state then attaches civil, criminal, and disciplinary penalties goes to another level entirely. Once having crossed that Rubicon, there is really no limit to state intervention in medical practice or the autonomy of physicians and patients to seek the best treatments possible for the condition at hand.