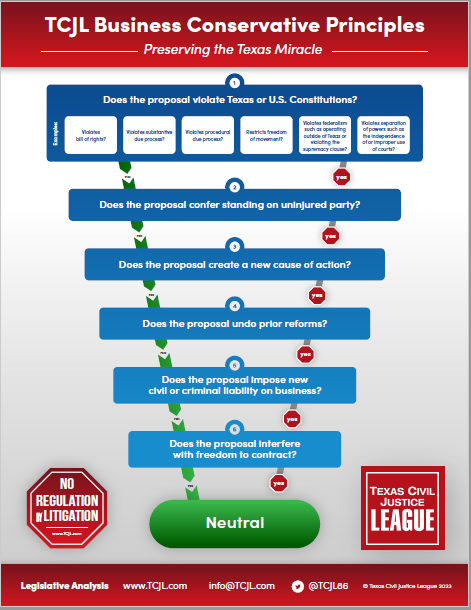
With the prefiling period for the 2021 legislative session only 10 days old, legislators have already filed more than 800 bills and resolutions. Bills filed so far indicate a broad range of policy priorities from both sides of the aisle, including pandemic response, Medicaid expansion, abortion regulation, public education, and police reform. Three important tort-related bills, however, have already been filed:
With the prefiling period for the 2021 legislative session only 10 days old, legislators have already filed more than 800 bills and resolutions. Bills filed so far indicate a broad range of policy priorities from both sides of the aisle, including pandemic response, Medicaid expansion, abortion regulation, public education, and police reform. Three important tort-related bills, however, have already been filed:
SB 207 by Schwertner. This proposed legislation amends §41.0105, CPRC, the paid or incurred rule enacted in 2003 to mitigate inflated health care expenses in personal injury and other litigation. Four years ago, TCJL, TLR, TADC, and other groups began to sound the alarm about an emerging practice in personal injury litigation: the use of letters of protection and other tactics designed to evade the paid or incurred rule. A letter of protection is an agreement between a plaintiff’s lawyer and a health care provider under which the provider agrees not to submit medical expenses to a third-party payor who may be obligated to pay those expenses in return for a promise to pay a higher amount out of an eventual settlement or judgment in the case. This arrangement allows the plaintiff’s lawyer to submit the full billed amount (the so-called “chargemaster” rate) as the amount “paid or incurred” for the claimant’s medical treatment.
Once submitted, the burden shifts to the defendant to prove that the rate is excessive, or, in other words, that it exceeds the reasonable and customary amount paid for the specific service in the area in which the service was provided. In order to prove that, the defendant must hire an expert and seek discovery of third-party reimbursement rates pertaining to the medical expenses involved in the case. Whether the defendant can actually get the information is another question altogether. Some trial judges may permit it, some may not. TCJL is aware of numerous cases, in fact, in which trial judges have denied such discovery and even stricken the defendant’s retained expert on medical billing, particularly if the expert was not a health care provider practicing in exactly the same field as the treating provider. In such cases, the defendant can only helplessly look on as chargemaster rates that nobody actually pays flow into evidence and end up in the jury room. Fortunately, two cases involving the striking of defense billing experts have made their way to the Texas Supreme Court, which is considering whether to grant review.
Among other things, the upshot of this situation is the revival of relatively low-dollar claims that otherwise would have been settled expeditiously under a proper application of the paid or incurred rule. But not only low-dollar claims. With the prospect of submitting into evidence significantly inflated expenses back in play, plaintiff’s lawyers have an incentive to take and file more cases. We can thus expect frequency and severity to start going up again after a period of relative stability. We can also expect defendants to reconsider whether to litigate claims where liability is a significant issue in light of the increased costs of discovery and higher exposure, particularly in urban trial courts roiled by mass turnover in recent elections. If this practice continues to spread, the paid or incurred rule will become a dead letter, eliminating a foundational part of the 2003 medical and general liability reforms.
SB 207 addresses these practices by allowing the defendant to introduce evidence of the reasonableness of the amount charged by a medical or health care service provided to a claimant, including:
- the amount actually paid to the provider for the service (unless there is a formal or informal agreement that the provider will wholly or partly refund, rebate, or remit the amount paid to the payer or another person);
- the amount billed by the provider; the amount paid, would have been paid, or likely to be paid for the services by a health benefit plan, workers’ compensation insurance, an employer-provided plan, Medicaid, Medicare, or other similar source;
- the average amount typically paid or allowed by health benefit plans or government payers to providers located in the same geographic area as the provider and who offer the same type of services as provided to the claimant; or
- the average amounts actually accepted in the 12 previous months by the provider for the same services provided to the claimant to patients other than the claimant.
TCJL strongly supports Senator Schwertner’s legislation, which will close the paid or incurred loophole.
HB 359 by Geren. This bill, which passed the House last session, overrules the Texas Supreme Court precedent of Brainard v. Trinity Universal Ins. Co., 216 S.W.3d 808 (Tex. 2006). The court ruled that an underinsured motorist (UIM) carrier is under no contractual duty to pay benefits until the insured obtains a judgment establishing the liability and underinsured status of the other motorist. Neither a claim nor a suit triggers a contractual duty to pay. Attorney’s fees and interest are not due until after the legal determination and damages are defined and upon a failure to pay by the carrier after proper presentment. The logic of the decision is perfectly sound: an insurer should not pay under a policy until the conditions precedent of the contract have been fulfilled. In the case of UM or UIM coverage, those conditions are whether the other motorist is one: (1) liable; and (2) actually uninsured or underinsured. HB 359 eliminates those requirements and legislative rewrites UM and UIM policies.
HB 501 by Wu: This legislation, which has been introduced in each of the past several sessions, indexes the caps on noneconomic damages and the amounts of required financial responsibility in health care liability claims, beginning in 2003. The effect of the bill would be to increase the current $250,000 cap on noneconomic damages in health care liability claims to approximately $1.8 million. TCJL will continue to oppose this bill. It will undermine the successful 2003 medical liability reforms that have increased access to health care in all areas of the state.