Employee Retirement Income Security Act of 1974
The Employee Retirement Income Security Act of 1974 (ERISA) is a federal law that sets minimum standards for most voluntarily established retirement and health plans in private industry to provide protection for individuals in these plans.
SB 1122 Died on Senate Intent Calendar TLO
ERISA Joint Association letter 4-26-25
 Loading...
Loading...
Federal District Court Rules That ERISA Preempts Tennessee Statute Requiring Health Plans to Accept Any Willing Provider for Pharmacy Benefits
ERISA Joint Association letter 3-20-25
 Loading...
Loading...
ERISA Joint Association letter 3-1-25
 Loading...
Loading...
Oppose ERISA Healthcare Mandates (SB 1122)
 Loading...
Loading...
Schwertner letter to Governor 2-10-25 Re: ERISA SB 2211
SB 1122 by Schwertner relating to applicability of certain prescription drug insurance laws to health benefit plans and pharmacy benefit managers.
 Loading...
Loading...
ERISA Joint Association letter to Governor 2-5-25
 Loading...
Loading...
AG Opinion KP-0480 2-5-25 Re: ERISA
 Loading...
Loading...
ERISA logo letter 2-3-25
 Loading...
Loading...
ERISA logo letter 10-31-2024
 Loading...
Loading...
TCJL Brief in Response to RQ-0539-KP Re: ERISA
 Loading...
May 22, 2024
Loading...
May 22, 2024
 Loading...
Loading...
TAHP Brief in Response to RQ-0539-KP Re: ERISA
June 17, 2024
 Loading...
Loading...
TAB Brief in Response to RQ-0539-KP Re: ERISA
June 17, 2024
 Loading...
Loading...
Senator Schwertner AG Opinion Request RQ-0539-KP Re: ERISA
May 13, 2024
RQ-0539-KP
During the 2023 legislative session, legislation (HB 2021) was introduced requiring a pharmacy benefit manager (PBM) contracted to administer a self-funded, employer-sponsored employee benefit plan governed by the Employer Retirement Income Security Act of 1974 (ERISA) (29 U.S.C. § 1001 et seq.) to comply with certain state statutes and regulations, If it had passed, HB 2021 would have certainly faced a legal challenge over whether it crosses the line into federal preemption territory. At the time, while we cautioned that it is always treacherous to try to predict what a federal court might do if presented with a challenge to this or similar legislation, we strongly asserted our opinion that HB 2021 crossed that line. On August 15, 2023, the U.S. 10th Circuit Court of Appeals, considering similar legislation enacted by the Oklahoma Legislature in 2019, confirmed that opinion.
In Pharmaceutical Care Management Association v. Glen Mulready, in his official capacity as Insurance Commissioner of Oklahoma; Oklahoma Insurance Department (No. 22-6074; filed August 15, 2023), the 10th Circuit reviewed an Oklahoma federal district court decision holding that certain requirements of the “Oklahoma’s Patient’s Right to Pharmacy Choice Act,” Okla. Stat. tit. 36, § 6958 et seq., escaped ERISA pre-emption. Among other things, the statute regulates the relationship between a PBM and its network pharmacists, prohibits a PBM from restricting an individual’s choice of an in-network pharmacy, bars a PBM from requiring an individual to use an affiliated pharmacy, and requires a PBM to meet certain access standards. The district court held that none of these changes had a “connection with” an ERISA plan because they did not “interfere with plan design or administration.” Rather, the provisions “may alter the incentives and limit some of the options that an ERISA plan can use, [but] none of the provisions force[d] ERISA plans to make any specific choices.” PCMA appealed the court’s decision to the 10th Circuit Court of Appeals. Several states, including Texas, joined in an amicus curiae brief defending the Oklahoma statute. The United States filed an amicusbrief taking the position that ERISA pre-emption applied.
In an opinion by Judge Gregory A. Phillips, joined by Senior Judge Michael R. Murphy and Judge Veronica S. Rossman, the court reversed the district court. Under 29 U.S.C. § 1144(a), ERISA pre-empts “any and all state laws insofar as they may now or hereafter relate to any employee benefit plan.” A state law “relates” to an ERISA plan if it has “(1) a ‘connection with’ or (2) a ‘reference to’ an ERISA plan” (citing Rutledge v. Pharmaceutical Care Management Association, 141 S. Ct. 474, 479 (2020), which involved a challenge to a 2015 Arkansas statute that required pharmacy benefit managers (PBMs) to reimburse pharmacies at or above the pharmacies’ cost to obtain a covered drug from a wholesaler). As SCOTUS likewise reminded everyone in Rutledge, “two categories of state laws [] have this impermissible connection with ERISA plans: ‘laws that require providers to structure benefit plans in particular ways, such as by requiring payment of specific benefits or by binding plan administrators to specific rules for determining beneficiary status,’ and laws whose ‘acute, albeit indirect, economic effects . . . force an ERISA plan to adopt a certain scheme of substantive coverage.” 141 S. Ct. at 480. In other words, the question is whether the state law “govern[s] a central matter of administration or interfere[s] with a nationally uniform plan administration”?
Noting that PCMA made only the “connection with” argument (the Oklahoma law, like HB 2021, assiduously avoided a direct “reference” to ERISA plans), the court first turned to Oklahoma’s argument that ERISA did not pre-empt the statute “because it regulates PBMs, not health plans.” In other words, the state asserted, since “PBMs are not plans, nor fiduciaries to plans” and such “plans need not contract with PBMs,” ERISA did not apply. This argument, which in our mind is naïve at best and disingenuous at worst, did not persuade the court. First, nothing in ERISA jurisprudence says that a state law has to expressly attack ERISA plans in order to invoke pre-emption. Rather, the inquiry goes to “the nature of the effect of the state law on ERISA plans” (citing Cal. Div. of Lab. Standards Enf’t v. Dillngham Constr., N.A., 519 U.S. 316, 325 (1997)), whether it “nominally” regulates them or not. Second, SCOTUS has explicitly held that “state laws can relate to ERISA plans even if they regulate only third parties.” In illustration, the 10th Circuit summarized two SCOTUS decisions, Metropolitan Life Insurance Co. v. Massachusetts, 471 U.S. 724 (1985) (holding that a state law requiring insurers to provide mental health benefits was subject to ERISA) and Rush Prudential HMO, Inc. v. Moran, 536 U.S. 355 (2002) (holding that a state law regulating HMOs was subject to ERISA). Third, the court had no trouble finding that the logic of these decisions squarely applies to PBMs. Observing that PBMs administer pharmacy benefits for about 270 million Americans and that, at the admission of Oklahoma’s pharmacist expert, pharmacies commonly rely on PBMs for up to 95% of their business, the court concluded that “[b]ecause a plan’s choice between self-administering its benefits and using a PBM ‘is in reality no choice at all,’ regulating PBMs ‘function[s] as a regulation of an ERISA plan itself’” (citations omitted).
The question then became whether the Oklahoma statute “preclude[d] the ability of plan administrators to administer their plans in a uniform fashion.” Specifically, the court examined the law’s “network restrictions,” which include access standards, discount prohibition, and any willing provider provisions, and its “integrity and quality restriction,” that is a probation provision. Briefly, the access standards require a PBM to construct its pharmacy network so that most enrollees reside within a certain number of miles of a preferred pharmacy, based on whether they live in urban, suburban, or rural areas. They also bar a PBM from using mail-order pharmacies to meet the standards. The discount prohibition blocks a PBM from offering cost-sharing discounts, such as reduced copayments, to incent enrollees to use in-network pharmacies. The any willing provider provision requires a PBM to accept any pharmacy into its preferred provider network if it agrees to network terms. Finally, the probation provision blocks a PBM from denying, limiting, or terminating a pharmacy’s contract because one of its pharmacists is on probation with the State Board of Pharmacy.
The court determined that ERISA pre-empts each of these provisions because each goes directly to benefit design, a “central matter of plan administration.” Regarding the network restrictions, the court looked to decisions from the 5thand 6th Circuits that rejected any willing provider laws on the basis that “ERISA plans that choose to offer coverage by PPOs are limited by the statute to using PPOs of a certain structure—i.e., a structure that includes every willing provider” (citing CIGNA Healthplan of La., Inc. v. Louisiana ex rel. Ieyoub, 82 F.3d 642 (5th Circ. 1996). In other words, the court observed, “the law prohibited ERISA plans from choosing a PPO that did not include all willing providers.” In response to Louisiana’s argument that its law did not mandate PBMs to use PPOs, the 5th Circuit replied that “Louisiana’s law ensured that ERISA plans that chose to use a PPO had to ‘purchase benefits of a particular structure,’ so it was pre-empted.” Oklahoma’s network restrictions similarly foreclosed an employer’s option to “choose a PPO that did not include all willing providers.” As the 10th Circuit opinion puts it, “the network restrictions mandate benefit structures; they at least ‘eliminate[] the choice of one method of structuring benefits.”
Specifically, the court ruled, the Oklahoma law’s access standards, any willing provider provisions, and discount prohibitions work together to “either direct[] or forbid[] an element of the plan structure or benefit design,” i.e., the scope of the pharmacy network and differential cost-sharing for the benefit of enrollees (even the State of Oklahoma was forced to admit this). The court looked at the implications of the case from a broader perspective as well. “Consider how the network provisions change the landscape for PBM networks in Oklahoma,” the court posed. “Before the Act, PBMs could use mail-order pharmacies to serve rural Oklahomans and reduce plan costs. Now, to comply with the Access Standards, PBMs working for Oklahoma plans with rural-dwelling employees must include many more brick-and-mortar pharmacies. Because adding pharmacies costs plans money, this is a choice that plans might not otherwise make.” The court made a similar point regarding the any willing provider provisions, which it observed would functionally collapse a two-tiered system designed to save employers and enrollees money to a one-tiered system that would cost everybody more money. In the words of the court, “[e]ach network restriction winnows the PBM-network design options for ERISA plans, thereby hindering those plans from structuring their benefits as they choose.” The court likewise determined that the probation provision was pre-empted because it requires a plan to accept allpharmacists into its network, even those subject to state discipline. When coupled with the any willing provider provision, the probation provision dictates which pharmacies must be included in the network, just like the network restrictions.
The court easily distinguished the Rutledge decision. “Unlike Arkansas’s reimbursement-rate regulations,” the court wrote, “Oklahoma’s network restrictions do more than increase costs. They home in on PBM pharmacy networks—the strcutures through which plan beneficiaries access their drug benefits. And they impede PBMs from offering plans some of the most fundamental network designs, such as preferred pharmacies, mail-order pharmacies, and specialty pharmacies.” The court dismissed out-of-hand various arguments advanced by the State of Oklahoma, to wit: the network restrictions are “narrower than they seem” (how?); the restrictions also apply to non-ERISA plans (as if that excuses the law from pre-emption); since ERISA doesn’t contain network restrictions, the state can impose them; the restrictions do not require plans to provide any particular benefits (it just takes away those benefits). The court did not belabor any of these because, candidly, they’re simply not serious legal arguments based on the pre-emption jurisprudence. The very brevity of the 10th Circuit’s discussion of them speaks volumes.
HB 2021 would have created exactly the same situation. By eliminating cost-sharing discounts and other incentives to use affiliated providers (or really event communicating with enrollees about it), restricting the use of mail-order pharmacies, effectively establishing a single-tier network, and requiring plans to accept pharmacists subject to state discipline, the bill would have forced employers into (more expensive) plan choices that they would otherwise have made. This employer choice is the quintessence of ERISA, which, after all, is designed to permit employers the most cost-effective benefit packages for their employees. Restricting those choices and running up the cost of ERISA plans, which HB 2021 would and bills like it would certainly do, undermine the whole purpose of ERISA. We said that during the session, and thanks to the 10th Circuit, we have a federal appellate decision directly on point saying the same thing.
We hope that this decision puts to rest efforts to revive HB 2021 or similar legislation in future sessions. It remains to be seen whether the State of Oklahoma will take the decision up to SCOTUS, but in view of the large number of states with an interest in the issues, it seems likely. In that event, we will await a definitive decision of the highest court in the land.
HB 2021: ERISA Logo Letter to House Insurance
March 27,2023
HB2021 Letterv3 (2) (31)
As you may recall from our prior analysis, HB 2021 would require a health benefit plan issuer or pharmacy benefit manager (PBM) contracted to administer a self-funded, employer-sponsored employee benefit plan governed by the Employer Retirement Income Security Act of 1974 (ERISA) (29 U.S.C. § 1001 et seq.) to comply with certain state statutes and regulations found in Chapter 1369, Insurance Code. Our analysis attempted to break the bill down into pieces and look at which individual provisions in Chapter 1369, as applied to ERISA plans, might survive a pre-emption challenge and which might not.
This afternoon at House Insurance Committee’s hearing on HB 2021, a proposed committee substitute was offered that substantially narrows the scope of the bill. Instead of bringing ERISA plans wholly under Chapter 1369, as the introduced version of the bill does, the substitute limits state regulation of ERISA plans to two subchapters. We discussed these, as well as the others, in our initial analysis, but since the bill now focuses on them, let’s take another look.
Our analysis will appear confusing because, as we noted previously, Chapter 1369 has two Subchapter Ls with the same section numbering. As luck would have it, CSHB 2021 targets these two, so we bear with us as we try to distinguish them without creating more confusion than already exists.
The first Subchapter L was added in 2021 by HB 1763. It governs the contractual relationship between plan issuers or PBMs and pharmacies or pharmacists and:
- prohibits an issuer or PBM from reducing the amount of a claim payment to a pharmacist or pharmacy after adjudication of the claim through the use of an aggregated effective rate, quality assurance program, or other direct or indirect remuneration fee except in accordance with an audit (§ 1369.553);
- bars a PBM from paying an affiliated pharmacist or pharmacy a reimbursement amount that is more than the amount the PBM pays a nonaffiliated pharmacist or pharmacy for the same service (§ 1369.555);
- prohibits an issuer or PBM from, as a condition of a contract, barring a pharmacy or pharmacist from sending an enrollee’s drugs by mail under certain circumstances (§ 1369.557);
- prohibits an issuer or PBM from requiring a pharmacy or pharmacist to meet accreditation or recertification standards more stringent than or inconsistent with federal and state requirements or blocking the dispensing of drugs that may be dispensed under the pharmacy’s or pharmacist’s license (§ 1369.558); and
- and prohibits retaliation against a pharmacy or pharmacist (§ 1369.559).
The second Subchapter L was likewise added in 2019 by HB 1919. This subchapter:
- blocks a plan issuer or PBM from transferring to or receiving from the issuer’s or PBM’s affiliated provider a record containing patient- or prescriber-identifiable information for a commercial purpose (§ 1369.553);
- steering or directing a patient to use an affiliated provider through online messaging regarding the provider or other advertising, marketing, or promotion of the provider (§ 1369.554); and
- prohibits an issuer or PBM from requiring a patient to use an affiliated provider to receive the maximum benefit or reduced cost-sharing and from soliciting a patient or prescriber to transfer a patient’s prescription to an affiliated provider (§ 1369.555).
The first question we ask is whether these provisions resemble those at issue in Rutledge v. Pharmaceutical Care Management Association, 141 S.Ct. 474 (2020), in which SCOTUS upheld an Arkansas statute over an ERISA pre-emption challenge brought by the Pharmaceutical Care Management Association (PCMA) on the basis that the statute merely established a floor for the cost of benefits that a plan may choose to provide, which may indirectly increase the cost of pharmacy benefits but does nothing to interfere with plan design or administration. The Court thus drew a clear line between legislation that deals with contracts between PBMs and in-network pharmacies and legislation that crosses the line into direct regulation of plan benefits or how the employer chooses to structure those benefits. As we noted in our prior analysis, Chapter 1369 contains provisions that in some ways parallel the Arkansas statute, but they are located primarily in Subchapter H, which deals with the use of formularies, maximum allowable cost lists, and pharmacy appeals of MAC prices. Consequently, it appears to us that the targeted subchapters in CSHB 2021 are not the same as those allowed through the pre-emption portal in Rutledge.
The question then becomes whether the provisions described above cross the pre-emption line because they interfere with the design or administration of an ERISA plan. The first Subchapter L clearly limits the ability of a health plan issuer or PBM to contract with pharmacies and pharmacists. It intervenes specifically, for example, in claims payment after an adjudication process, differential treatment of affiliated and nonaffiliated providers, and accreditation and recertification standards. These do not seem to be matters confined solely to a “floor for the cost of benefits that a plan may choose to provide,” as SCOTUS ruled in Rutledge. Instead, they establish what is permissible in a contract between a health plan and a provider or between a health plan and a third-party administrator. In our view, these provisions have a significant impact on both plan design and administration to the point of directly affecting prescription drug benefits, the specific terms under which they can be offered to enrollees, and the specific methods and procedures through which a health plan or administrator determine an whether claims have been paid appropriately. We think a very strong argument can be made that this part of CSHB 2021 is likely pre-empted.
The same goes with applying the second Subchapter L to ERISA plans, this time with regard to regulating the communications between the plans and their enrollees about their providers. In particular, among other things, it blocks a health plan from offering a plan design that: (1) confers a higher benefit if an enrollee uses the plan’s affiliated provider; (2) provides for reduced cost-sharing if an enrollee uses the plan’s affiliated provider; and (3) informs an enrollee of the enrollee’s option to transfer a prescription to an affiliated provider. These kinds of contractual arrangements would appear to go to the heart of plan design, since they determine the level of benefits, not just the cost of benefits, and the contractual relationship between the health plan issuer and the enrollee. To us, this is a bridge too far into pre-emption territory.
In an important sense, HB 2021 has little to do with pharmacies and pharmacists, and everything to do with the impingement of state regulation on ERISA plans more generally. If the changes proposed by the bill can be applied to ERISA prescription drug benefits, they can be applied to all benefits and all providers. And at that point, the primary benefit of ERISA—to promote private health insurance coverage by making it easier for employers to provide uniform coverage for employees wherever located—will be destroyed.
Recently introduced legislation would require a pharmacy benefit manager (PBM) contracted to administer a self-funded, employer-sponsored employee benefit plan governed by the Employer Retirement Income Security Act of 1974 (ERISA) (29 U.S.C. § 1001 et seq.) to comply with certain state statutes and regulations, The legislation, HB 2021, sets up a potential clash over whether it crosses the line into federal preemption territory. It is always treacherous to try to predict what a federal court might do if presented with a challenge to this or similar legislation, but there are at least two recent decisions that may indicate the current judicial thinking on ERISA and PBM regulation.
Before getting into the big question, however, let’s take a look at what HB 2021 purports to do. The bill adds a new section to Subchapter D, Chapter 4151, Insurance Code, which requires pharmacy benefit managers to issue identification cards to enrollees and prohibiting them from selling a list of patients that contains information through which the identity of an individual patient is disclosed. That subchapter further requires a PBM to maintain the confidentiality of patient information unless disclosure is authorized by law or by the patient. The new subsection, § 4151.155, states that a PBM “must comply with the provisions of Chapter 1369 with respect to each plan administered by the [PBM], regardless of whether a provision of that chapter is specifically made applicable to the plan” (italics added). As you might have guessed, the italicized language refers to ERISA plans that contract with PBMs for third-party administration of prescription drug benefits. The bill goes on to exempt a PBM from complying with a provision of Chapter 1369 “(1) with respect to a plan expressly excluded from the applicability of the provision; or (2) to the extent that the commissioner [of insurance] determines that the nature of third-party administrators renders the provision inapplicable to [PBMs].”
Chapter 1369, Insurance Code, broadly regulates a health benefit plan’s coverage of prescription drugs, devices, and related services. It applies to a health benefit plan that “provides benefits for medical or surgical expenses incurred as a result of a health condition, accident, or sickness,” which includes individual and group policies. § 1369.002. The following section lists the types of health benefit plans not subject to Chapter 1369, but this list does not specifically exempt ERISA plans. We presume that, unless ERISA plans are exempted elsewhere in Chapter 1369, HB 2021 brings those plans under the general regulatory umbrella that applies to other employee health benefit plans provided by insurance carriers and other licensed issuers.
The next step in the analysis is to determine which provisions of Chapter 1369, if applied to an ERISA plan, raise a preemption concern. The only part of Chapter 1369 that explicitly excludes “a self-funded health benefit plan as defined by [ERISA]” is Subchapter F, which regulates the manner in which a PBM may audit a pharmacy or pharmacist. As noted above, the rest of the chapter would presumably apply to an ERISA plan by virtue of HB 2021 unless pre-empted. As we have previously reported, a pair of recent federal court decisions address ERISA preemption of state regulations of PBMs. HB 2021 undoubtedly stems from these decisions at least in part, so it is important that we look closely at them in attempt to distinguish which provisions of Chapter 1369 might pass muster and which won’t.
The leading case is Rutledge v. Pharmaceutical Care Management Association, 141 S.Ct. 474 (2020), which arose from a 2015 Arkansas statute that required pharmacy benefit managers (PBMs) to reimburse pharmacies at or above the pharmacies’ cost to obtain a covered drug from a wholesaler. This law required PBMs to update their lists specifying the maximum allowable cost (MAC) for each drug each time the wholesale price changed, established an appeals process for pharmacies challenging the amount of reimbursement, and increased the reimbursement rate if a pharmacy could not obtain the drug at a lower price than the MAC list specified from its customary wholesaler. If a pharmacy could not get reimbursement from a PBM at the price of acquisition or above, the pharmacy could decline to sell the drug to a beneficiary of the plan. SCOTUS upheld the Arkansas statute over an ERISA pre-emption challenge brought by the Pharmaceutical Care Management Association (PCMA) on the basis that the statute merely established a floor for the cost of benefits that a plan may choose to provide, which may indirectly increase the cost of pharmacy benefits but does nothing to interfere with plan design or administration. The Court thus drew a clear line between legislation that deals with contracts between PBMs and in-network pharmacies and legislation that crosses the line into direct regulation of plan benefits or how the employer chooses to structure those benefits.
The Arkansas statute at issue in Rutledge has some parallels in Chapter 1369. These include:
- 1369.354, which requires a plan issuer or PBM to use the FDA’s “Orange Book” to formulate MAC prices and to disclose to pharmacists and pharmacies the sources of the pricing data;
- 1369.355, which requires a plan issuer or PBM to establish, maintain, and frequently update MAC price information for each drug;
- 1369.356, which requires the issuer or PBM to provide ready access to the MAC list for pharmacists and pharmacies;
- 1369.357, which establishes a process by which pharmacists and pharmacies may appeal a MAC price; and
- 1369.402, which bars an issuer or PBM from directly or indirectly charging or holding a pharmacist or pharmacy responsible for any fee for any step or component related to a claims adjudication process.
It should be noted that legislation has also been filed to require a health benefit plan issuer to reduce an enrollee’s cost-sharing amount for prescription drugs by an amount equal to or greater than all rebates received or to be received from the enrollee’s PBM (HB 2180). If both this bill and HB 2021 make their way into law, this requirement will apply to ERISA plans as well.
As to HB 2021’s application of the above provisions to ERISA plans, what might the federal courts say? Like the Arkansas statute upheld in Rutledge, these provisions govern the relationship between PBMs and pharmacists and pharmacies, MAC prices, and the appeals process. So far, perhaps (we should never predict the courts), so good. But they also impose pricing requirements directly on plan issuers and, it seems to us, interfere with plan design and administration. Specifically, they require plan issuers to adopt certain pricing practices and regulate the relationship between issuers and enrollees. A very strong argument can thus be made that, at least as to the application of HB 2021 to this part of Chapter 1369, the bill is pre-empted.
Moreover, as we have described, HB 2021 draws ERISA plans into Chapter 1369 in other ways as well. We have noted that the only Subchapter F, Chapter 1369, which provides for audits of pharmacies and pharmacists, explicitly exempts ERISA plans. We have further discussed the effect of the bill on Subchapter H (MAC prices) and Subchapter I (pharmacy benefit claims adjudication). What about the rest of Chapter 1369? Let’s take it subchapter by subchapter.
- Subchapter A requires a health benefit plan that covers prescription drugs to cover any drug prescribed to treat an enrollee for a chronic, disabling, or life-threatening illness covered under the plan if the drug has FDA approval and or is otherwise validated by the commissioner peer-reviewed medical literature. It further prohibits from denying coverage based on “medical necessity” unless the reason for the denial is unrelated to the legal status of the drug use. § 1369.004. Finally, the subchapter caps the amount that a plan issuer may require an enrollee to pay for a prescription drug at the point of sale and requires the plan to allow refills of prescription eye drops under certain circumstances. § 1369.0041.
- Subchapter B: prescribes requirements for plan issuers regarding notices to enrollees of drug formularies (§ 1369.054); limits the time and manner of modifications of drug coverage under a plan (§ 1369.0541); imposes guidelines that a plan issuer must follow when requiring a step therapy protocol (§ 1369.0545); mandates that an issuer establish a process under which a provider may request an exception to a step-therapy protocol, and deems such a request as granted under certain circumstances (§ 1369.0546); requires an issuer to offer an enrollee continuing coverage of a drug removed from the formulary until the plan renewal date (§ 1369.055); and makes the refusal of an issuer to provide coverage for a prescription drug not included in a formulary and determined by the enrollee’s physician to be medically necessary as an adverse determination (§ 1369.056).
- Subchapter C prohibits a plan from excluding or limiting benefits for an FDA-approved prescription contraceptive drug or device (§ 1369.104) or imposing a cost-sharing requirement for such drugs or devices or an outpatient contraceptive service more than the amount required for other benefits (§ 1369,105). It further limits waiting periods for contraceptive drugs, devices, or outpatient services (§ 1369.106) and prohibits a plan from discriminating against an enrollee because of the enrollee’s use of a contraceptive drug, device, or outpatient service (§ 1369. 107).
- Subchapter D prescribes required content for enrollee identification cards (§ 1369.153).
- Subchapter E mandates coverage for a prescribed, orally administered anticancer medication and limits cost-sharing to the same basis as chemotherapy treatment. It further bars an issuer from reclassifying anticancer medications or increasing cost-sharing requirements without also applying the same increases to the majority of comparable medical or pharmaceutical benefits under the plan (§ 1369.204).
- Subchapter E-1 prohibits an issuer that covers stage-four advanced, metastatic cancer and associated conditions from requiring an enrollee to fail to respond to a different drug prior to covering a prescribed drug (§ 1369.213).
- Subchapter G directs the commissioner to prescribe a single, standard form for prior authorization of prescription drug benefits, requires issuers to use the form and to make it available on various websites, and penalizes issuers for failing to accept the form (§ 1369.304).
- Subchapter J requires a plan to prorate any cost-sharing amount charged for a partial supply of a prescription drug used to treat a chronic illness based on the necessity of synchronizing the dates that the pharmacy dispenses the enrollee’s prescription (§ 1369.454), bars the issuer from prorating a fee paid to the pharmacy for dispensing a drug for which cost-sharing was prorated (§ 1369.455), and mandates that the plan establish a process through which the plan, the enrollee, the enrollee’s provider, and the pharmacist may jointly approve a medication synchronization plan, which must include certain circumstances under which the pharmacist may override the plan (§ 1369.456).
- Subchapter K requires PBMs to file annual reports with the commissioner stating the aggregated rebates, fees, price protection payments, and any other payments collected from pharmaceutical drug manufacturers and the amount of those payments passed on to health benefit plan issuers or enrollees at the point of sale of the drug (§ 1369.502). It further requires the issuer to submit the names of the 25 most frequently prescribed drugs across all plans, the percent increase in annual net spending and premiums for drugs across all plans, the percent of specialty drugs with utilization management requirements across all plans, and the premium reductions attributable to specialty drug utilization management (§ 1369.503).
- Subchapter L governs the relationship between plan issuers or PBMs and pharmacies or pharmacists. It prohibits an issuer or PBM reducing the amount of a claim payment to a pharmacist or pharmacy after adjudication of the claim through the use of an aggregated effective rate, quality assurance program, or other direct or indirect remuneration fee except in accordance with an audit (§ 1369.553). It further bars a PBM from paying an affiliated pharmacist or pharmacy a reimbursement amount that is more than the amount the PBM pays a nonaffiliated pharmacist or pharmacy for the same service (§ 1369.555); prohibits an issuer or PBM from, as a condition of a contract, barring a pharmacy or pharmacist from sending an enrollee’s drugs by mail under certain circumstances (§ 1369.557), prohibits an issuer or PBM from requiring a pharmacy or pharmacist to meet accreditation or recertification standards more stringent than or inconsistent with federal and state requirements or blocking the dispensing of drugs that may be dispensed under the pharmacy’s or pharmacist’s license (§ 1369.558), and prohibits retaliation against a pharmacy or pharmacist (§ 1369.559).
- Subchapter L (yes, there are two subchapter Ls with the same section numbers) blocks a plan issuer or PBM from transferring to or receiving from the issuer’s or PBM’s affiliated provider a record containing patient- or prescriber-identifiable information for a commercial purpose (§ 1369.553) or steering or directing a patient to use an affiliated provider through online messaging regarding the provider or other advertising, marketing, or promotion of the provider (§ 1369.554). Finally, an issuer or PBM may not require a patient to use an affiliated provider to receive the maximum benefit or reduced cost-sharing, nor to solicit a patient or prescriber to transfer a patient’s prescription to an affiliated provider (§ 1369.555).
Interestingly, the companion bills SB 1221 and HB 826 make several changes to Subchapter B, Chapter 1369, which include new notice requirements for health benefit plan issuers if they increase an enrollee’s prescription drug costs and a prohibition of modifying, on renewal of a policy, an enrollee’s contracted benefit level for a previously covered prescription drug for a medical condition or mental illness that the prescribing physician determines is the most appropriate course of treatment. Contrary to HB 2021, these bills specify that ERISA plans are excluded from Subchapter B, undoubtedly because they directly “interfere with plan design or administration.”
Regarding the remaining subchapters, it seems reasonably clear that A, C, E, and E-1 mandate that health benefit plans provide benefits for specified conditions. Applying these requirements to ERISA plans, in our view, would likely be pre-empted because they go to the heart of plan design and would compel ERISA plans to offer benefits in Texas that might not be available in other states (though nothing prevents ERISA plans from offering the mandated benefits). Subchapter B broadly regulates drug formularies and would appear to breach ERISA pre-emption by imposing non-uniform plan administration requirements. Subchapter D, requiring uniform pharmacy benefit cards, may or may not implicate ERISA pre-emption to the extent it requires Texas enrollees to have different cards than enrollees in other states (we’re not sure how significant an impact on plan administration this might be). We have already seen that Subchapter F explicitly exempts ERISA plans and would not be affected by HB 2021, but Subchapter G, which requires standard forms for requesting prior authorization forms, would be. We are certainly not in the business of administering ERISA plans, but it seems to us that using a different form for this purpose in Texas than in other states could produce a significant administrative and compliance headache. The same goes for Subchapter I, which directly infringes plan administration by imposing specific limitation on the administration of the claims adjudication process. We think Subchapter J would most likely fail the pre-emption test because it micromanages the costs and medication synchronization plans, hitting both plan design and administration. The first Subchapter L would seem to present a better case for avoiding pre-emption, as it simply requires an annual report, but the same might not be true for the second Subchapter L. That one goes directly to plan design and administration in its regulation of the plan’s contracts with affiliated providers, levels of payment to affiliated and nonaffiliated providers, and communications with prescribers and enrollees.
To summarize this long, frequently tedious, but nevertheless necessary analysis, we have a high level of confidence that HB 2021 has very significant ERISA pre-emption implications. If enacted, there is no question that litigation would ensue, with a reasonable probability that the bill’s attempt to apply Subchapters A, C, E, E-1, G, I, J, and the second L to ERISA plans would fail. Again, we will leave it to the real experts on ERISA pre-emption to tell us if they agree or disagree with us, and—as always—we both stand to be corrected and never purport to predict what a court will do.
As we have previously reported, legislation seeking to impose mandates or otherwise change the benefit structure of self-funded employer-sponsored health benefit plans (“ERISA” plans) threatens to undermine those plans by subjecting them to state-by-state regulation. To date, the United States Supreme Court has repeatedly ruled that such efforts are pre-empted by federal law. Despite this long line of authority, proponents of imposing state regulation on ERISA plans are looking to two recent cases for evidence that the federal courts are loosening the standards for states seeking to pierce ERISA pre-emption. A closer reading of these cases, however, reveals that they do nothing of the sort and that there is little to no indication that SCOTUS is ready to lift the pre-emption bar.
Both of the cases involve the relationship between pharmacy benefit managers (PBMs) and retail pharmacies. The first, Rutledge v. Pharmaceutical Care Management Association, 141 S.Ct. 474 (2020), arose from a 2015 Arkansas statute that required pharmacy benefit managers (PBMs) to reimburse pharmacies at or above the pharmacies’ cost to obtain a covered drug from a wholesaler. This law required PBMs to update their lists specifying the maximum allowable cost (MAC) for each drug each time the wholesale price changed, establish an appeals process for pharmacies challenging the amount of reimbursement, and increase the reimbursement rate if a pharmacy could not obtain the drug at a lower price than the MAC list specified from its customary wholesaler. If a pharmacy could not get reimbursement from a PBM at the price of acquisition or above, the pharmacy could decline to sell the drug to a beneficiary of the plan. SCOTUS upheld the Arkansas statute over an ERISA pre-emption challenge by the Pharmaceutical Care Management Association (PCMA) on the basis that the statute merely established a floor for the cost of benefits that a plan may choose to provide, which may indirectly increase the cost of pharmacy benefits but does nothing to interfere with plan design or administration. The Court thus drew a clear line between legislation that deals with contracts between PBMs and in-network pharmacies and legislation that crosses the line into direct regulation of plan benefits or how the employer chooses to structure those benefits.
Last spring an Oklahoma federal district court reached a similar conclusion in Pharmaceutical Care Management Association v. Glen Mulready, in his official capacity as Insurance Commissioner of Oklahoma, and the Oklahoma Insurance Department (Case No. CIV-19-977-J; filed April 4, 2022). In 2019 the Oklahoma Legislature enacted the “Oklahoma’s Patient’s Right to Pharmacy Choice Act,” Okla. Stat. tit. 36, § 6958 et seq. Among other things, the statute regulates the relationship between a PBM and its network pharmacists, prohibits a PBM from restricting an individual’s choice of an in-network pharmacy, bars a PBM from requiring an individual to use an affiliated pharmacy, and requires a PBM to meet certain access standards. The district court held that none of these changes have a “connection with” an ERISA plan because they do not “interfere with plan design or administration.” Rather, the provisions “may alter the incentives and limit some of the options that an ERISA plan can use, [but] none of the provisions forces ERISA plans to make any specific choices.” PCMA has appealed the court’s decision to the 10thCircuit Court of Appeals. A number of states, including Texas, have joined in an amicus curiae brief defending the Oklahoma statute. As was the case in Rutledge, this Oklahoma statute deals solely with the contractual relationship between PBMs and in-network pharmacies.
These decisions neither break legal precedent nor herald a paradigm shift in the way SCOTUS evaluates ERISA pre-emption claims. While we are cognizant and appreciative of the Legislature’s desire to reduce health care costs, regulating ERISA plans will do far more harm than good. Not only would employers have to comply with 50 different state regulatory regimes mandating different plan benefits and administrative requirements, but they would be placed in a position in which employees in some states got “better” benefits than those in others. The disruption this would likely cause to an employer’s workforce is hard to predict, but the concern is real. While any Texas legislation in this arena will certainly be litigated to the bitter end, inviting such litigation will significantly detract from the legislative policies that have made the Texas economy the most dynamic and successful in the nation.
The Case for Preserving ERISA
January, 2023
by Lee Parsley, TLR, January 2023
https://www.tortreform.com/advocate/tlr-advocate-january-2023/
The Employee Retirement Income Security Act of 1974 (ERISA) allows multistate employers to design health and retirement benefit plans tailored to their workforces and to administer those plans uniformly across the nation.
In creating ERISA, Congress recognized that multistate employers cannot provide quality, affordable healthcare benefits and retirement plans to employees if they must comply with a patchwork of recordkeeping and reporting requirements—or multiple state and local mandates—in addition to complying with federal laws.
Uniformity encourages employers to offer health and retirement plans to employees, thus reducing the number of uninsured Texans and increasing the number of people who can retire without excessive reliance on government support.
ERISA comprehensively regulates the administration of employee healthcare plans that provide “medical, surgical, or hospital care or benefits, or benefits in the event of sickness, accident, disability [or] death.” It does not regulate the substantive content of such plans. Thus, each employer can choose for itself the costs and benefits that best fit its circumstances.
ERISA guarantees uniformity by preempting any state or local law that “relates to” an employee benefit plan governed by ERISA. Preemption of state laws is allowed by the Supremacy Clause of the U.S. Constitution (Art. VI, cl. 2), which comes into play when state law conflicts with valid federal law.
The Supremacy Clause should be viewed in context with the Tenth Amendment of the Constitution, which explicitly states that powers not delegated to the federal government by the Constitution are reserved to the states or the people. Courts have determined that ERISA is a valid federal statute pursuant to the Commerce Clause of the Constitution and, thereby, is a law that can properly preempt conflicting state or local laws.
The preemption rule in the ERISA statute expressly prohibits states and localities from forcing employers to create or amend an ERISA-sanctioned employee benefit plan, or from enacting statutes or ordinances controlling the administration of an employee benefit plan established under ERISA.
ERISA preemption matters for two reasons. First, it allows companies that operate across state lines to establish uniform health plans for their entire workforces. Second, entrepreneurial plaintiff’s lawyers seek to end ERISA preemption for their personal gain.
Texas’ Prompt Payment of Claims Act (PPCA) governs payments by insurance companies to healthcare providers. It is the most punitive law of its kind in the nation and, thus, can be richly profitable to lawyers who file late-payment lawsuits.
So profitable, in fact, that several years ago, numerous Texas lawyers solicited hospitals and doctors to sue insurance companies for alleged failures to timely reimburse them for patient services. In fact, one of Texas’ wealthiest personal injury trial lawyers sent a letter to virtually every licensed attorney in the state claiming to have developed a computer algorithm that would identify late payment of claims. He asked all Texas lawyers to refer their doctor and hospital clients to him to pursue PPCA lawsuits for a share of the profits.
Because of this activity by profit-seeking lawyers, PPCA lawsuits were filed in courthouses across Texas seeking tens of millions of dollars in penalties. To the extent these lawsuits succeeded, Texas consumers paid the price in the form of higher insurance premiums—another “Tort Tax” buried in the cost of a necessary product.
Courts, however, eventually held that the PPCA is preempted by ERISA. Consequently, health insurance companies who manage employer-provided healthcare plans and the employers who pay for these benefits for their employees are not currently subject to PPCA lawsuits. This literally saves Texans millions of dollars.
But the trial lawyers’ quest for enrichment has not ended. They want the Legislature to pierce ERISA’s preemption, opening ERISA to mandated coverages, rate setting by governmental functionaries (rather than negotiated rates between the provider and insurer) and PPCA lawsuits. These lawyers would like to pursue PPCA lawsuits and personal injury lawsuits arising from alleged denials of benefits and breaches of fiduciary duty.
Ending or eroding ERISA preemption will adversely impact labor markets, disadvantage employees based on where they live or work, cause employers to cut back on benefit coverage and raise the cost of health insurance and retirement plans.
The Texas Legislature should protect ERISA preemption, not weaken it.
Several bills that already been introduced that raise serious questions about ERISA preemption. Brief summaries of the bills are as follows. We have highlighted the provisions that, in our view, may have ERISA implications. Disclaimer: we are flagging these bills so that our members who have ERISA plans may study them further and inform us as to their potential ramifications. We will do our best to spot as many of them as we can, but please let us know if we miss something!
- We have high confidence that HB 307 and HB 404 are pre-empted because they mandate that an employer provide a benefit that the employer is not required to provide in other jurisdictions.
- HB 494, which creates an employer-funded wage replacement fund, appears similar to local ordinances in California and elsewhere that require employers to “pay-to-play” in providing minimum benefits. These types of mandates have been challenged, but SCOTUS has yet to consider them.
- HB 1032, SB 304, and SB 308 appear to mandate restrictions on benefits provided by employer-sponsored health plans that differ from other jurisdictions.
HB 307 by Bernal (D-San Antonio): Adds Chapter 83, Labor Code, to require employers to provide paid sick leave annually.
HB 404 by Collier (D-Dallas): Requires private employers to provide paid leave annually. Requires employers with 75 or fewer employees to provide paid leave after the second anniversary date of the date the employer hires its first employee. Provides that paid leave accrues at one hour for each 30 hours worked up to a maximum of 40 hours per calendar year. Entitles an employee to carry over 40 hours of unused leave to the next year, unless the employer pays the employee for the unused leave or offers the full amount of leave expected to accrue in the following year. Requires an employee to work at least 18 hours a week to use paid leave. Prohibits an employer from taking an adverse employment action against an employee who requests or uses paid leave or who files a complaint with the TEC. Imposes an administrative penalty of $500 for a violation involving retaliation against an employee, $100 for other violations. Imposes liability on an employer of employee who prevails in a civil action for lost wages, salary, benefits, or other compensation, as well as equitable relief, including reinstatement or promotion. Allows the court to award reasonable attorney’s fees, expert witness fees, and other costs to the employee.
HB 494 by Meza (D-Irving): Entitles an employee who has worked for an employer for at least one year to up to 30 days of leave to attend to the employee’s own serious health condition or the serious health condition of the employee’s spouse, child, grandchild, sibling, parent, parent-in-law, grandparent, or grandparent-in-law. Also extends to the birth of a child or care or services necessary if the employee or member of the employee’s family are a victim of family violence, sexual assault or abuse, stalking, or trafficking. Does not require leave to be paid but entitles the employee to wage replacement benefits for leave taken. Provides that if the employer offers paid leave, an employee is entitled to the average amount that would have been paid to the employee during the pay period. Does not entitle an employee to accrual of seniority or other employment benefits during the leave period or any right, benefit, or position the employee was not previously entitled to. Creates a wage replacement benefit fund funded by employee contributions of .25% of the employee’s monthly pay. Makes violations of this chapter unlawful employment practices.
HB 1032 by Noble (R-Allen): Adds Subchapter N, Insurance Code, to prohibit a group health benefit plan issuer or a life insurance company from using an individual’s COVID-19 vaccination status to discriminate against the individual in providing coverage. Purports to preempt any other law. Amends Chapter 21, Labor Code, to prohibit an employer from discriminating against a person who has not received a COVID-19 vaccination. Immunizes an employer from suit arising from a failure to mandate a COVID-19 vaccine. Prohibits an elementary or secondary school or institution of higher education from discriminating against a student who has not received a COVID vaccination. Blocks HHSC from adding COVID-19 to the list of mandatory vaccinations.
SB 304 by Hall (R-Edgewood): Prohibits a person from discriminating against or refusing to provide a public accommodation based on the person’s vaccination history or immunity status for a communicable disease. Enforceable by the attorney general in a suit for equitable relief. Prohibits such discrimination by a long-term care facility, health care provider, health care facility. Punishes violations by defunding, disciplinary action, and administrative penalties. Prohibits a health benefit plan from discriminating against an individual based on vaccination status. Prohibits a health benefit plan from using an individual’s vaccination status in rating. Prohibits a health benefit plan from discriminating against a provider based on the vaccination status of the provider’s patients. Prohibits an employer from discriminating against an individual based on vaccination status. Prohibits a licensing agency from discriminating against a licenseholder or applicant based on vaccination status. Prohibits an educational institution, hospital, or health care facility from requiring as a condition of employment to be vaccinated or to participate in vaccine administration. Creates a private right of action for equitable relief, reinstatement, back pay, and interest. Prohibits TXDOT from discriminating against a driver’s license applicant based on vaccination status. Abolishes vaccination requirements for schools and institutions of higher education. Eliminates emergency authorization for a physician to administer a vaccination. Bars disciplinary action against child care providers or foster parents for declining to immunize a child. Bars the state or a local government from requiring vaccines. Bars a health care provider from disclosing a person’s vaccination history. Abolishes all child vaccine requirements.
SB 308 by Hall (R-Edgewood): Prohibits a person from discriminating against or refusing to provide a public accommodation based on the person’s COVID-19 vaccination history or immunity status for a communicable disease. Enforceable by the attorney general in a suit for equitable relief. Prohibits such discrimination by a long-term care facility, health care provider, health care facility. Punishes violations by defunding, disciplinary action, and administrative penalties. Prohibits a health benefit plan from discriminating against an individual based on COVID vaccination status. Prohibits a health benefit plan from using an individual’s vaccination status in rating. Prohibits a health benefit plan from discriminating against a provider based on the COVID vaccination status of the provider’s patients. Prohibits an employer from discriminating against an individual based on COVID vaccination status. Prohibits a licensing agency from discriminating against a licenseholder or applicant based on COVID vaccination status. Prohibits an educational institution, hospital, or health care facility from requiring as a condition of employment to be vaccinated for COVID or to participate in vaccine administration. Creates a private right of action for equitable relief, reinstatement, back pay, and interest. Prohibits TXDOT from discriminating against a driver’s license applicant based on COVID vaccination status. Abolishes vaccination requirements for schools and institutions of higher education. Eliminates emergency authorization for a physician to administer a COVID vaccination. Bars disciplinary action against child care providers or foster parents for declining to immunize a child for COVID. Bars the state or a local government from requiring COVID vaccines. Bars a health care provider from disclosing a person’s COVID vaccination history.
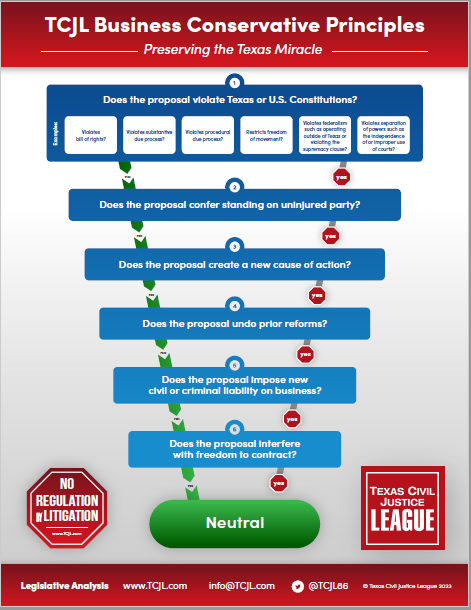
In the wake of SB 8, we expect to see numerous bills filed this session to challenge federal preemption of state and local laws and regulations that interfere with self-funded employer-sponsored benefit plans (so-called “ERISA” plans). We have prepared the attached primer on ERISA for purposes of evaluating specific legislative proposals and their potential effects on employers that provide ERISA plans. TCJL will vigorously oppose proposals that challenge preemption and undermine the stability and uniformity of ERISA plans.
 Loading...
Loading...