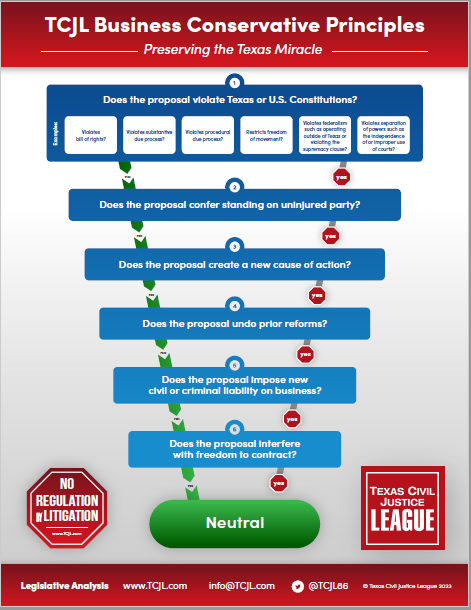
On April 5, 2023, we posted an analysis of several bills that expanded the liability of health care providers so significantly that we questioned whether the Legislature was undoing the immense progress Texas has made since 2003 in enhancing access to health care by placing rational limits on medical liability. Nearly two years on, at the beginning of the 2025 legislative session, we find ourselves asking the same question—and bill filing has barely even started.
On April 5, 2023, we posted an analysis of several bills that expanded the liability of health care providers so significantly that we questioned whether the Legislature was undoing the immense progress Texas has made since 2003 in enhancing access to health care by placing rational limits on medical liability. Nearly two years on, at the beginning of the 2025 legislative session, we find ourselves asking the same question—and bill filing has barely even started.
Specifically, two of the more problematic proposals that did not pass last session have reappeared. The first, SB 619, appears to be the same bill introduced in 2023 as HB 319. The proposal:
- allows a person to decline to participate in a health care service for reasons of conscience, subject to exemptions for emergency care or, except as otherwise by Chapter 166, Health and Safety Code, life-sustaining treatment;
- grants immunity from civil or criminal liability for a physician or health care provider who declines to participate in a health care service wholly or partly for reasons of conscience;
- prohibits a person from taking adverse action against another person because the person declines to participate in a health care service for reasons of conscience, including licensure, certification, employment, staff appointments or privileges, and various other actions;
- requires a health care facility to develop a written protocol for circumstances in which a person declines to participate in providing a health care service;
- bars the protocol from requiring a health care facility, physician, or health care provider to counsel or refer a patient to another physician or facility;
- establishes a complaint process at the appropriate licensing agency; and
- creates a private cause of action for injunctive relief, actual damages for “psychological, emotional, and physical injuries resulting from a violation of this law,” court costs, and attorney’s fees.
The bill’s statement of purpose maintains that the law is needed to protect health care providers from being forced to violate their beliefs by rendering health care services that they do not find “morally acceptable.” Aside from questions of whether this proposal comports very well with a physician’s Hippocratic Oath or medical ethics more generally, it raises very significant liability concerns—and not only because it creates a private cause of action for, among other things, “psychological” and “emotional” injuries (how in the world can one quantify an injury to one’s “conscience” anyway?). (Presumably, under the bill a physician could sue a hospital or another physician simply for arguing with a provider who invokes this statute about the ethical issues involved in “declining” to participate in the treatment of a patient.)
There is an even more serious practical concern, however. The proposal grants immunity from civil and criminal liability to a provider who declines to participate in treating a patient for reasons of conscience. Suppose a physician or other provider objects to a patient’s religious affiliation (or lack thereof) or some other aspect of the patient’s identity, which may include anything from the patient’s race or nationality, immigration status, gender expression or sexual preference—the list goes on. The bill further refers to refusal to treat based on a “moral philosophy or ethical position” without regard to a particular religious position. Does that mean, for example, if a patient espouses capitalist views, a provider who prefers a socialist “philososophy” can simply opt out? Whatever the reason for discriminating based on one’s “conscience,” does the immunity in the bill override all other anti-discrimination laws? The answer has to be yes, since the conscientious objector “may not be held civilly or criminally liable” for declining to participate in the treatment of a patient.
But an even more insidious aspect of the proposal is that it leaves everyone else holding the bag. While the conscientious objector gets off scot-free, somebody presumably will provide the withheld treatment. Suppose the objector bails out of a complex case with multiple complications (that doesn’t rise to the level of requiring emergency life-sustaining care). Now suppose that while the hospital is scrambling to find another provider with the necessary expertise to treat that case, the patient gets worse and suffers harm as a result of the delay. Who pays for that? The hospital? The nurses who tried to manage the situation when the objector walked away? The physician who ended up trying to restore the deteriorating condition the objector left behind? How will this possibility even be insured? And by the way, the proposal requires a health care facility to adopt a written protocol for handling this situation but at the same time bars the protocol from counseling or referring a patient to another facility or physician that may be able to provide better treatment, or at least somebody willing to treat the patient!
What seems to be forgotten in this type of approach is the individual in need of medical treatment. Isn’t that ill or injured human being the pre-eminent concern of medical practice? That would seem to be the focus of another bill, SB 754. A version of this bill, too, was filed last session, but it pertained only to COVID-19 vaccinations. The present version has been expanded to any health care service. It does the following:
- prohibits a health care provider from coercing or compelling an individual lawfully residing in Texas into obtaining a health care service contrary to the individual’s preference (but an individual “unlawfully” residing in Texas);
- requires a provider to obtain informed consent before providing a health care services to a lawful resident (an individual coerced or compelled to receive a service is not considered to have capacity to consent);
- prohibits a person from taking an adverse action against a person who refuses or fails to obtain a health care service, including a vaccine;
- exempts a person employed, working in, or training in a health care facility from receiving a health care service if the person orally or in writing requests an exemption based on a sincerely held religious belief or a recognized medical condition for which the service is contraindicated;
- authorizes the attorney general to obtain injunctive relief, investigative costs, attorney’s fees, witness fees, and despostion expenses to enforce the statute
- creates a private cause of action for a civil penalty of not less than $5,000 plus investigative costs, attorney’s fees, witness fees, and despostion expenses to a prevailing party;
- provides an affirmative defense if the individual stated to the practitioner in advance of the service that consent was voluntarily provided.
This proposal appears to place an individual’s medical treatment explicitly in the individual’s own hands, which on its face is not a bad thing. And requiring that a health care provider to inform a patient of what the provider, in the provider’s medical judgment, thinks is necessary and obtaining a patient’s free and voluntary consent to treatment seems like a good idea. The problem is, how does a health care provider really know what a patient’s “preference” is? For that matter, how does a patient know what the patient’s preference is if the patient has no medical training? Presumably, one goes to the doctor because a doctor has the education, training, and expertise to treat the ailment or injury. A patient with a gangrenous foot may “prefer” that the doctor not amputate the foot, but if patient “prefers” to survive, the foot has to be amputated. The proposal attempts to cover this (admittedly extreme) situation by providing that a doctor’s “advice” or “recommendation” in itself does not constitute “coercion” or “compulsion,” but that’s cold comfort to the doctor faced with a patient that simply refuses life-saving treatment because he or she “prefers” something else. In other words, at what point does “advice” or “recommendation” become coercive?
This is not to say that a patient shouldn’t be able to make the final choice when presented with the alternatives, but the patient isn’t the only player in the game. What about the patient’s family? If grandpa comes in to the hospital with a gangrenous foot but won’t hear of having the foot amputated, who bears the risk of the ensuing complications, potentially including grandpa’s horrible and painful death from sepsis? Well, clearly the doctor whose advice was ignored, the hospital, and the hospital staff will. This bill may even set up the possibility that the doctor can be sued both for “coercing” grandpa to have his foot amputated and for neglecting to amputate it! Think of the position in which this bill puts a health care practitioner in the case where a family has conflicting “preferences” about what ought to be done.
There are other problems, but you get the idea. Proposals of this kind introduce an enormous degree of uncertainty into the risk profile of practicing medicine. The more liability roadblocks the Legislature puts between a health care practitioner and a patient will eventually have serious effects on access to quality health care in the state, if it is not already doing so (and there is evidence that it is). We can well imagine a physician coming off the grueling experience of medical school and residency into a liability environment that has as many pitfalls as these and other proposals (we’ll get to some of them later) will create.
We’ve gotten used attractive practice environment for health care providers that the 2003 medical liability reforms established. If we undo it piece-by-piece in this fashion, we’ll have only ourselves to blame if we wake up in ten years without enough of them who are willing to take the risk of putting down roots here.